The Gender Gap
Cardiovascular disease (CVD) or Coronary Artery Disease (CAD) is the leading cause of death in North America. North American women are 10 times more likely to die from heart disease than from breast cancer. In spite of this unmistakable risk to women, heart disease remains almost invisible to us. In a 1997 study released by the American Heart Association, published in the Lancet – only 8% of women recognized that heart disease and stroke were their leading cause of death – responsible for deaths of more women each year than the next 16 causes of death combined (causes include everything from diabetes, ALL forms of cancer and AIDS to accidents).1 One reason may be, as we know, that symptoms of heart disease, congestive heart failure and heart attacks in women differ from those in men. The familiar heart attack symptom of crushing pain in the chest and left arm is more common in men than women. Heart attack symptoms are vastly different for women where the primary signs of a heart attack are usually unrelated to chest pain. They include some of the following:
- discomfort in the neck, shoulder, upper back or stomach
- shortness of breath
- pain in one or both arms
- nausea
- sweating
- dizziness
- profound fatigue
- an impending sense of doom
For a visual – I regularly use and adore this clip in really bringing the message home. I find it to be an excellent example of how commonly women and physicians may dismiss symptoms. Please view this 3min 41sec video here:
For a moving personal story from a 41 year-old women who survived a heart attack, Please view this 6min 37sec video here:
In 2003, the National Institute of Health (NIH) and the American Heart Association, (AHA) embarked on national campaign to educate women about heart disease. While we are still struggling to understand gender-specific differences, it does seem that women are more prone to the impacts of inflammation and hormonal imbalances, and those are the drivers for women’s cardiovascular disease.
What I often see in pre- and peri-menopause is that women develop insulin resistance that progresses overtime – not necessarily to frank diabetes – but towards obesity, hyperlipidemia, elevated blood pressure, and the inability to lose weight. A lot of the insulin resistance is mediated hormonally on a local tissue level. Understanding and addressing these hormone imbalances is an important step in women’s heart health and cardiovascular risk reduction.
I will come back to the topic of hormones a little later in this article.
Current Standard of Care – Falling short
Our current screening methods for heart disease in men, but especially in women, fall short of good prevention strategies. Heart disease is a long haul game and we need to start our prevention as early as possible. While we base risk factors on a 10-year risk for cardiovascular disease such as the Framingham Risk Assessment tool (originating from the 1970’s, I might add), as our standard of care – it really ought to be updated & more proactive. Why not look at 30 years or more? Even as early as the teens and twenties, we start developing plaque build-up in our arteries. It is a slow process that develops over many decades. Here are some statistics:
- Up to 30% of young males (ages 16 to 20 years old) who died a premature death from motor vehicle accidents, homicides and non-heart related deaths already had atherosclerotic lesions or plaques in their coronary arteries upon autopsy findings.2
- Bioidentical Estrogen Replacement Therapy (BHRT) or Hormone Replacement Therapy (HRT) reduces the risk of heart disease in women – when started early (at the onset of menopause)
- Risk of heart disease in women rises dramatically after menopause.
- 50% of heart attacks occur before the age of 65 years old.
Clarity on cholesterol – Breaking down it’s bad reputation
Cholesterol often gets a bad rap. But cholesterol is essential to life. We need cholesterol to produce some of the most important structures in the body like cell membranes, hormones (including testosterone, progesterone, estrogen, and cortisol) and bile acids – necessary to digest our food and activate our thyroid functions.
The standard cholesterol panel is simply not good enough. We cannot anticipate heart disease risk and start early prevention on these parameters alone. The standard lipid panel includes: Total cholesterol, LDL cholesterol, non-HDL cholesterol, HDL cholesterol, and triglycerides. While they serve as a guide, there is more to understand.
We generalize that having higher levels of HDL – known as the “good” cholesterol, is healthy and can offset LDL, otherwise referred to as the “bad” cholesterol. While it is important to screen these markers – further understanding and evaluation is needed.
It’s not the cholesterol that is necessarily good or bad, rather, it is what they are transported by. It is more about the “cargo ships” that carry the cholesterol that increases the risk and formation of plaque build-up inside the vessel walls. The cargo ships that carry the “good” HDL particles and the “bad” LDL particles are different. Most notably, standard screening tests fail to measure this. So let me break it down for you:
Apolipoprotein A (ApoA) is a protein involved in lipid metabolism, mainly associated with high-density lipoproteins (HDL). HDL particles – the “good” cholesterol – tagged with ApoA are able to cross the endothelial barrier (the semipermeable layer between the vessel lumen – inside of the blood vessel – and the arterial wall). HDL particles do this easily and have the following benefits:
- Cross the endothelial barrier easily for lipid transport back and forth
- HDL lowers inflammation and maintains the integrity of the endothelium
- HDL acts as an arterial antioxidant by neutralizing and stopping the oxidation of LDL
- HDL can arrive at a “fatty streak” or foam cell and suck cholestereol back out from a macrophage in a process called “de-lipidation.” It then slips back into the blood stream and transports the excess cholesterol to the liver and other tissues for re-use – known as the Cholesterol Efflux. This is a good thing and reduces cholesterol burden in the blood vessel wall.
Apolipoprotein B (ApoB) is a protein involved in lipid metabolism, mainly associated with low-density lipoproteins (LDL), very low-density lipoproteins (VLDL’s), triglycerides and Lipoprotein(a). ApoB is a key component in assessing cardiovascular risk, as elevated levels are shown to increase the risk of plaque build-up in the arterial walls. ApoB particles are the more specific measurement for “bad cholesterol” and here is why:
- LDL particles with their larger tagged ApoB carrier are bigger molecules and can get “stuck” in the endothelium and then become “oxidized.” Two factors that we know of which further increase oxidation in the blood vessel wall include high blood pressure and smoking. High blood pressure causes mechanical damage, where smoking causes chemical damage and both increase the retention of LDL into the blood vessel wall and create greater oxidation and inflammation.
- The immune system responds to inflammation in the endothelium by sending monocytes (large white blood cells) to confront the oxidized aggregate of ApoB tagged cells. These turn into macrophages to gobble up the LDL, the way a Pacman might, in an attempt to reduce the damage and remove the bad cholesterol from the arterial wall. But if it too much cholesterol is consumed, then it can blow up into a foam cell. And this is the beginning of a fatty streak – where the arterial plaque is born.
Why else is ApoB screening important? A paper published in JAMA Cardiology in 2021 found that each standard deviation increase in ApoB raises the risk of myocardial infarction (the clinical term for a heart attack) by 38% without a history of cardiac event or diagnosis of cardiovascular disease.3 However, in 2024 the standard lipid panel screening has not evolved. I strongly recommend adding ApoB testing as a preventive measure to gage a persons’s level of cardiovascular risk.
Lipoprotein(a) or LP(a) is a particle similar to LDL but with an additional protein. Elevated LP(a), otherwise called “el-pee-little-a” is a deadly type of LDL lipid that can contribute to a higher risk of cardiovascular disease, particularly in familial cases.
- This is the most prevalent hereditary risk factor for heart disease and it is still flying under the radar of general conventional medicine.
- Elevated Lipoprotein(a) is associated with increased coagulation and a one-to-three times increased incidence of CVD. Lp(a) has been linked to the promotion of both early and advanced staged atherosclerosis.4
- Lp(a) is dangerous based on its larger, more irregular shape. This LP(a) protein wraps loosely around an LDL particle with large looping amino acid segments called “kringles” because it looks like the Danish pastry. As the kringles pass through the blood stream, they scoop up bits of oxidized lipid molecules, amongst other things, and carry them along.
- While there may be some positive cleansing that happens along the ride of the blood vessel wall, their potential to permeate into the endothelium and get lodged in the arterial wall is high risk.
- Lipoprotein(a) is thus far more likely than a simple LDL to get stuck in the arterial wall -with all the oxidized bits of cholesterol it picked up along the way – and then act as a thrombotic or pro clotting factor – faster and meaner than a regular LDL particle.
If there is a family history of parent, grandparent or aunt/uncle – or perhaps all 3 – who died of premature heart disease, then you should be asking for a Lipoprotein(a) blood test. Because this is a largely genetic test, it only needs to be done once. And contrary to the comments below on statin medications, in cases of high Lipoprotein(a) – it is one of the few treatments available to reduce overall risk.
Homocysteine (HCy) is yet another marker on blood work that can be used to evaluate heart disease risk. Homocysteine is an amino acid where high levels of homocysteine (HCy) are toxic to vascular endothelial cells and may also be directly neurotoxic (implicated in conditions like Alzheimers Disease).5,6 Homocysteine may be elevated as a result of genetics, methylation defects, hypochlorhydria (not enough stomach acid production), or other causes and can and easily be added to a lipid panel blood test.
Screening for these important subset of cholesterol & genetic markers is an important step to comprehensivly evaluating your risk for heart disease. Using these screening tools, alongside Healthy Lifestyle Practices are a critical step in the prevention of cardiovascular disease.
Statin Medications
Contrary to popular medical belief, Statin drugs should not be prescribed to everyone who has high cholesterol. To be clear, I am not against prescribing statin drugs, but they must be prescribed with caution, understanding, and appropriateness. Common side effects from statin medications such as Lipitor, Crestor and the like, are not trivial and can include:
- liver enzyme abnormalities
- muscle weakness and pain – most commonly the hamstring, quadriceps and calves.
- Severe muscle pain – known as rhabdomylosis – where the muscle cells breakdown, necrose (and die) as a direct result of Statin Therapy.
- joint pain
- onset of diabetes in some individuals
- Cardiomyopathy & heart failure is a known risk factor 7
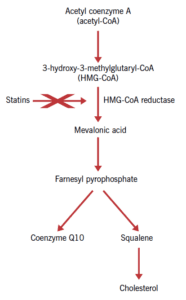
Every knowledgeable doctor should recommend that every patient take the critical vitamin Co-Enzyme Q10 alongside every statin prescription. The problem is, most doctors are not knowledgeable in the importance of CoEnzyme Q10 to help offset some of these symptoms. Statin drugs stop the body from making this critical skeletal and cardiac muscle nutirent, in addition to reducing cholesterol 7. In some cases, even the co-administration of CoEnzyme Q10 may fail to alleviate the side effects of statin therapy.
Synthetic pathway for Coenzyme Q10 Source: British Journal of Cardiology 8
3 Common Myths about Statins & Cholesterol you need to know
Myth 1 – High total cholesterol and high LDL numbers are the number 1 cause of heart disease in North America
Wrong. High total cholesterol is among the many risk factors for heart disease, but it is not the leading cause. The most prevalent risk factor is actually low HDL along with small LDL particles, which commonly occur together. In fact, for those with coronary heart disease, 60-70 percent will have low HDL and small LDL particles, but fewer than 30 percent will have high LDL.9,10,11,12 Truth be told, it’s just not as profitable for drug companies to sell high quality food: almonds, walnuts, Omega 3 oils, fibre and other natural agents. That is not to say they haven’t tried – it just does not generate the revenue of a statin drug.
There are multiple risk markers for atherosclerosis and cardiovascular disease and in combination, they create greater inflammation in the body. The following risk factors identified for coronary heart disease and arterial damage include:
- High CRP
- High LDL
- Excess insulin
- Low HDL
- High blood sugar
- Nitric oxide deficit
- High triglycerides
- Low free testosterone
- Excess fibrinogen
- Excess homocysteine
- High blood pressure
- Low Vitamin K
- Excess cholesterol.
Myth 2: If I take a statin agent, I won’t have a heart attack.
Also untrue. Lowering your cholesterol levels to within range, reduces, but does not eliminate, the risk of heart attacks. Many heart attacks still occur in people with low cholesterol levels, whether or not they take cholesterol-lowering drugs.13 This is where speaking with your doctor about healthy lifestyle habits and screening for the higher risk genetic markers can help.
Myth 3: I feel fine. My stress test was normal. My doctor says I don’t have heart disease.
Inaccurate. Haven’t you heard? Heart Disease is a silent killer. Most future deaths and heart attacks actually occur in people with normal stress tests.14
Better screening tests include a calcium score of the coronary arteries or the even more accurate CT angiogram which will pick up the more dangerous soft plaques in addition to hard plaques.
While a CT angiogram is not an easy ask in our restrictive health care screening measures of BC, costs a bit more, requires IV dye and exposes a patient to slightly more radiation – it is the most sensitive means to evaluate risk. About 15% of people who have normal calcium scores are still found to have soft plaque or even small calcifications on CT angiograms. Further to this, as many as 2-3 % pf people with a zero calcium score are found on CT Angiogram to have high risk plaques.2
You can start your prevention for cardiovascular risk with healthy lifestyle habits, getting an up-to-date cholesterol panel and adding the more sensitive markers Apolipoprotein B (ApoB), Lipoprotein(a) and Homocysteine (HCy).
Back to the Gender Gap – Are Statins really the first best choice for women ?
Men and women are different and women are not simply smaller versions of men. Here is evidence of such difference when it comes to how we treat men versus women with high cholesterol levels and statin drugs. This exerpt is taken directly from Estrogen Matters, Chapter 3: Matters of the Heart:
When it comes to women, to assess the value of statins, a woman at risk of heart disease needs to know two things: (1) is high cholesterol on its own, a significant risk factor, and (2) do statins and lowering cholesterol, lower that risk? The answers are no and no.
In The Truth About Statins, cardiologists, Barbara H Roberts, Director of the Women’s Cardiac Centre at the Miriam Hospital in Providence, Rhode Island, reports that statins are less effective in women than men, that they have their greatest benefit in preventing a second heart attack, and that they are more of a marketing success story, than a medical one. 38 In a major review, supporting that conclusion, physicians, Judith Walsh and Michael Pignone found 13 studies of the effects of statins on women and men with and without cardiovascular disease. Six of these studies representing 11,435 women without cardiovascular disease, showed that lowering cholesterol levels, did not reduce overall mortality rates and did not lower the chances of having a non-fatal heart attack or other coronary heart disease symptoms. Eight studies representing 8,272 women who already had cardiovascular disease showed that statins did reduce the risk of non-fatal and fatal heart attacks. 39 Furthermore – and this finding always comes as a shock to people – there is no relationship between total cholesterol levels and death from heart disease, especially for women40.
(We are not talking about subtypes of cholesterol like LDL (Apo-B, LP (a) and triglycerides where high levels of which are risk factors).
Why a women should consider Estrogen (or Hormone) Replacement Therapy (ERT / HRT)?
Admittedly, the Women’s Health Initiative (WHI) generated a lot of controversy within the medical community with regards to hormone therapy and risk. Thus it has become easier for physicians to tell women they can’t take hormones because the study showed they were harmful. Unfortunately, the WHI was frought with false claims, an unhealthy population pool, and misrepresentation of the facts. I encourage every woman to read Estrogen Matters by Avrum Bluming and to make an informed decision for themselves. I will include a brief summation here.
Published in JAMA in 1997, in a randomized controlled trial in which 643 healthy post-menopausal women were divided according to time since menopause, under six years or more than 10 years, they were randomly assigned to receive either ERT (or HRT) or placebo. Every six months for an average of five years, the investigators measured the thickness of the woman’s carotid arteries – an indication of potential cardiovascular problems – and assessed the existence and degree of atherosclerosis with CT scans. HRT was responsible for significantly slower progression of atherosclerosis, as compared to placebo, but only when it was begun within six years of menopause. There was no benefit when it was initiated to 10 or more years after menopause.16
In summary, there is now a consensus, that when taken at the start of menopause, or before age 60, HRT, confers protection against coronary artery disease and heart attacks. Menopause is defined as the absence of periods for 12 months. But many women begin having menopause related symptoms – such as night sweats, weight gain, insomnia, muscle pains, and heart palpitations – even when they are still menstruating, and HRT can benefit them too. Here is what we know.
- ERT or HRT may have beneficial effects on the heart for women who start taking hormones early in menopause, because estrogen promotes healthy blood vessels, and may help delay the formation of plaque.
- ERT or HRT probably has no protective effect on women who begin the use of hormones later, in their mid 60s, or 10 years after menopause – although this conclusion is still being a evaluated.
- ERT or HRT is potentially risky for women who begin taking it in their 60s, at least for the first year especially if they have pre-existing coronary artery disease. This is due to the inflammatory effect of estrogen because it can create inflammation in existing arterial plaques – either causing a stable plaque to rupture or can promote bleeding into the plaque. After one year – this risk is no longer apparent. But I would be remiss to not mention, this one year risk is also equivalent to a women who happens to be sedentary, overweight or a smoker.
I understand the hesitation surrounding ERT, HRT and BHRT (it has many names). We have been misinformed by the misrepresentation of research that came out of the Women’s Health Initiative Trials.
Nananda Col and her colleagues conclude that hormone replacement therapy should increase life expectancy for nearly all post-menopausal women, with some gains exceeding three years, depending mainly on an individual‘s risk factors for coronary heart disease and breast cancer.49 It is important to mention that for women, with at least one risk factor for coronary heart disease, Hormone therapy should extend life expectancy, even for women having a first-degree relative with breast cancer. The benefit of hormone replacement therapy, and reducing the likelihood of developing CHD appears to outweigh the risk of breast cancer for all women in whom this treatment might be considered.17
Further to the 1997 analysis above, the American College of cardiology in 2017 at their annual meeting, reported their findings after analyzing the records of more than 4000 women. After adjusting for their ages, calcium scores, and cardiovascular risk factors, they found that women who had been taking HRT were
- 30% less likely to die than those not on hormone therapy.
- 36% less likely to have a coronary calcium score above 399, which is indicative of severe atherosclerosis, plaque buildup, and high heart attack risk, and
- 20% were more likely to have a coronary calcium score of zero, the lowest possible score, indicating a low likelihood of heart attack. 18
The evidence is clear, taking a statin is perhaps not the best first choice for women, when it comes to primary heart disease prevention. But if hormone replacement therapy can add 3 to 4 more years of healthy life with a much lower risk of heart disease and this is good enough for you – It’s good enough for me to prescribe it.
Prevention of heart disease is a complex subject. Lifestyle factors, statin medications, hormone replacement therapy are just a few considerations when it comes to taking care of your heart. There are many natural agents that we use in Naturopathic Medicine, from plant extracts such as Allium and Commiphora to Berberine and Red Yeast Rice. If it has been awhile since you have had a blood work up, a cholesterol panel and even a physical exam, we are happy to get you back on track for a healthy heart. Please contact our office.
Please note Naturopathic Doctors are able to provide primary care in the province of BC, provide physical exams, order blood work on your behalf and refill prescriptive medications if and when appropriate. While we are still lobbying with the government for expanded scope to have some of these services covered, to date our care remains an out-of-pocket expense and we do offer direct billing for our consultations, for those patients who do have extended health benefits.
References:
- Assessing the odds. Lancet 1997;350:1563.
- Attia, P & Gifford, B. Outlive: The Science and Art of Longevity. Chapter 7: The Ticker 2023 p. 122-124.
- Apo B – Marston et al. (2022) JAMA Cardiology in 2021
- Lp (a) – Pearson GJ, THanassoulis, G, Anderson TJ, et al. 2021. Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the preventions of cardiovascular disease in the adult . Can J Cardiol. 2021; 31:1129-1151.
- Seshadri S, Wolf PA, Beiser AS, et al. Association of plasma total homocysteine levels with subclinical brain injury: cerebral volumes, white matter hyperintensity, and silent brain infarcts at volumetric magnetic resonance imaging in the Framingham Offspring Study. Arch Neurol. 2008;65(5):642-649.
- Oulhaj A, Refsum H, Beaumont H, et al. Homocysteine as a predictor of cognitive decline in Alzheimer’s disease. Int J Geriatr Psychiatry. 2010;25(1):82-90.
- Langsjoen PH et al: Statin-Associated Cardiomyopathy Responds to Statin Withdrawal and Administration of Coenzyme Q10 Perm J 2019:23:18-257. doi: 10.7812/TPP/18.257. Epub 2019 Aug 26
- Image: David Mantle. Coenzyme Q10 and cardiovascular disease: an overview. October 2015Br J Cardiol 2015;22:160 doi:5837/bjc.2015.037
- Gardner CD et al: Association of small low-density lipoprotein particles with the incidence of coronary artery disease in men and women,JAMA Sep 18;276(11):875-81, 1996.
- Stampfer MJ et al: A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction,JAMA Sep 18;276(11):882-88, 1996.
- Lamarche B et al: Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men: Prospective results from the Quebec Cardiovascular Study,Circulation Jan 7;95(1):69-75, 1997.
- Kuller L et al: Nuclear magnetic resonance spectroscopy of lipoproteins and risk of coronary heart disease in the cardiovascular health study,Arterioscler Thromb Vasc Biol Jul 1;22(7):1175-80, 2002.
- van Lennep JE et al: Apolipoprotein concentrations during treatment and recurrent coronary artery disease events,Arterioscler Thromb Vasc Biol Nov;20(11):2408-13, 2000.
- Taylor AJ et al: 34th Bethesda Conference: Can atherosclerosis imaging techniques improve the detection of patients at risk for ischemic heart disease? J Amer Coll Cardiol Jun 4;(11)41:1860-2, 2003.
- Bluming, A & Tavris, C. Estrogen Matters: Why taking hormones in menopause can improve women’s well-being and lengthen their lives-without raising the risk of breast cancer. Chapter 3: Matters of the Heart 2018 – References from Exerpt taken from Estrogen Matters:
- B. H. Roberts, The Truth About Statins: Risks and Alternatives to Cholesterol Lowering Drugs (New York: Pocket Books: 2021) and H. Rosenberg and D. Allard, “evidence for Caution: Woman and statin use,” 2007. Women and Health Protection Report, Canada http://www.whpapsf.ca/pdf/statinEvidenceCaution.pdf
- Walsh JME. Pignone M. Drug treatment of hyperlipidemia in women. JAMA 2004;291:2243-52.
- G Taubes, The Case Against Sugar ( New York: Knopf, 2016)
- Hodis HN, Mack WJ, Henderson VW, et al. Vascular effects of early versus late postmenopausal treatment with estradiol. N Engl J Med. 2016;374:1221-31.
- Col NF, Eckman MH, Karas RH, et al Patient specific decisions about hormone replacement therapy in postmenopausal women. JAMA 1997;277:1140-47.
- Arnson Y, et al Hormone replacement therapy associated with lower mortality. Press release from the American College of Cardiology, March 8, 2017; https://eurekalert.org/pub_releases/2017-03/acoc-hrt030617.php







