Hot Flashes Could Signal Increased Risk for Heart Disease
 A new study finds that women who experience frequent hot flashes in younger midlife (age 40 – 53 years) may be more likely to have poor vascular function regardless of cardiovascular disease (CVD) risk factors or estradiol levels. These findings were published online April 12, 2017 in Menopause.
A new study finds that women who experience frequent hot flashes in younger midlife (age 40 – 53 years) may be more likely to have poor vascular function regardless of cardiovascular disease (CVD) risk factors or estradiol levels. These findings were published online April 12, 2017 in Menopause.
Researchers evaluated data from 272 nonsmoking women aged 40 to 69 years who were late perimenopausal (2 – 12 months amenorrhea) or postmenopausal (≥12 months amenorrhea).
All women underwent physical examinations, brachial artery flow-mediated dilation (FMD) to assess endothelial function, carotid artery ultrasound, blood draw, and ambulatory hot flash monitoring, using an electronic hot flash diary (3 days), a wrist actigraph (3 days), and a physiologic hot flash monitor (24 hours). Menopause status was assessed from reported menstrual bleeding patterns. Estradiol levels (E2), glucose, high-density lipoprotein cholesterol, triglycerides, total cholesterol, insulin, C-reactive protein, and interleukin 6 were evaluated.
Even after controlling for other CVD risk factors, younger women (aged 40 – 53 years) who experienced hot flashes had a lower blood flow (or FMD) compared with women who did not experience hot flashes, indicating poorer endothelial function.
There are natural ways, (herbal and nutrient-based) to balance your hormones and reduce your risk for heart disease. At the same time, you can rid yourself of these disruptive hot flashes and improve your sleep.
To find out how and learn more, book an appointment with Dr. Emina Jasarevic, ND.
(Excerpt: Source: http://www.medscape.com/viewarticle/878644 You don’t have access to this so I’ll include it below)
A new study finds that women who experience frequent hot flashes in younger midlife (age 40 – 53 years) may be more likely to have poor vascular function regardless of cardiovascular disease (CVD) risk factors or estradiol levels. These findings were published online April 12 in Menopause.
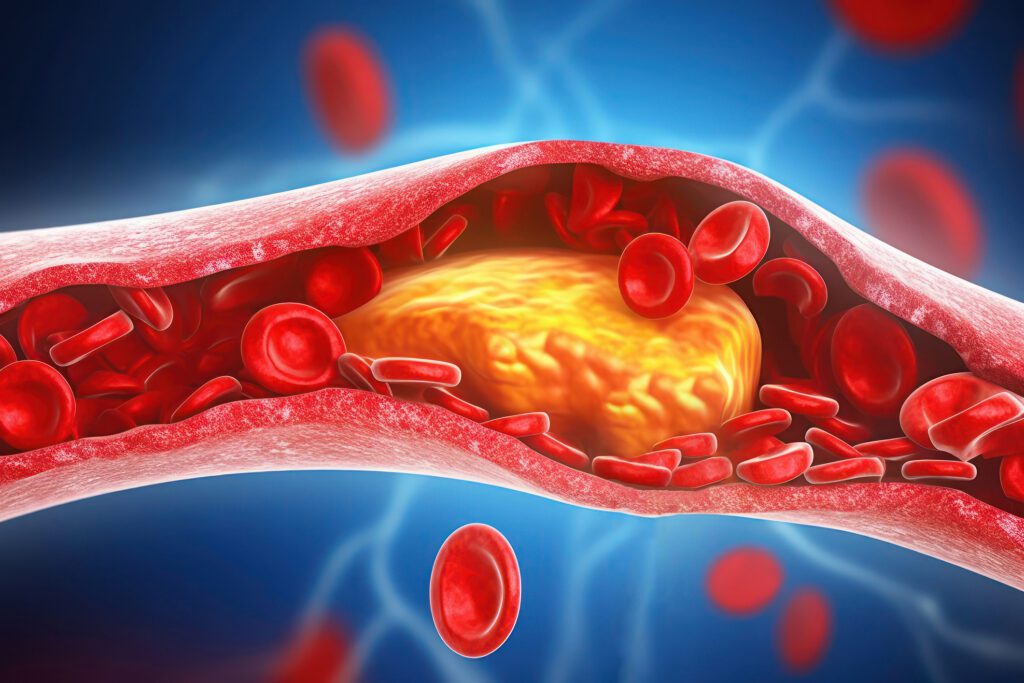
” Impairment in endothelial function is an initiating event in the atherosclerotic process, and thereby frequent hot flashes may mark emerging vascular dysfunction among early midlife women,” write Rebecca C. Thurston, PhD, from the University of Pittsburgh School of Medicine, Pennsylvania, and colleagues.
Researchers evaluated data from 272 nonsmoking women aged 40 to 69 years who were late perimenopausal (2 – 12 months amenorrhea) or postmenopausal (≥12 months amenorrhea). The study excludes women with CVD, neoplasia, hysterectomy, and/or bilateral oophorectomy, kidney failure, seizures, Parkinson’s disease, Raynaud’s phenomenon, or current pregnancy. The researchers also excluded women with a history of recent use of reproductive hormone agents, serotonin reuptake inhibitors, insulin, or cardiovascular drugs. On average, participants were 54 years of age, white, college educated, and postmenopausal and had a relatively favorable CVD risk factor profile.
All women underwent physical examinations, brachial artery flow-mediated dilation (FMD) to assess endothelial function, carotid artery ultrasound, blood draw, and ambulatory hot flash monitoring, using an electronic hot flash diary (3 days), a wrist actigraph (3 days), and a physiologic hot flash monitor (24 hours). Menopause status was assessed from reported menstrual bleeding patterns. Estradiol levels (E2), glucose, high-density lipoprotein cholesterol, triglycerides, total cholesterol, insulin, C-reactive protein, and interleukin 6 were evaluated.
Even after controlling for other CVD risk factors, younger women (aged 40 – 53 years) who experienced hot flashes had a lower FMD compared with women who did not experience hot flashes (P = .01), indicating poorer endothelial function.
Further, the investigators found that a greater frequency of physiologically monitored hot flashes was also associated with poorer FMD among this group (P = .03, multivariable). Notably, the authors point out that “the FMD of the youngest women with hot flashes was similar to the FMD of women in the oldest tertile [age 54 – 60 years].” There was no association between hot flashes and FMD found among older women.
With respect to the role of E2, the researchers found that levels were not significantly associated with FMD and did not lessen the association between hot flashes and FMD among younger women (40 – 53 years).
“The present study shows that menopausal hot flashes are associated with poorer endothelial function independent of E2 among younger women only,” write the authors.
The researchers note that previous studies have demonstrated an association between early-onset hot flashes and increased CVD risk and hypothesize that “different CVD markers may show different temporal relations to hot flashes, progressing from endothelial dysfunction to atherosclerosis to clinical CVD events,” although the pathophysiologic mechanism behind this association remains unclear.
The authors acknowledge study limitations such as the lack of data from early perimenopausal women or from women in racial/ethnic minority groups.
“These findings point to the potential value in considering the role of not only hormones, but also hot flashes, in the cardiovascular changes that occur early in the menopause transition, while also underscoring the potential role that the endothelium may play in the physiology of early hot flashes,” conclude Dr. Thurston and colleagues.
Funding for this study was provided by the National Institutes of Health, National Heart Lung and Blood Institute, and by the University of Pittsburgh Clinical and Translational Science Institute. The authors have disclosed no relevant financial relationships.
Menopause. Published online April 12, 2017. Abstract