“Truth is the daughter of time not of authority” – Francis Bacon.
Estrogen and Hormone Replacement Therapy (HRT) offer several significant health advantages, many of which extend beyond typical menopause symptom relief.
Here are the five key, surprising benefits:
- Estrogen reduces your heart disease risk by 50%
- Estrogen prevents and delays osteoporosis by 40%
- Taking HRT delays dementia in 40-50% of women
- Estrogen reduces your colon cancer risk by 30-50%
- HRT increases longevity & life span by a few years
For the last 2 decades – there has been a stubborn narrative that Hormone Replacement Therapy (HRT) is dangerous for your health. Specifically, that it puts you at a high risk for developing breast cancer and heart disease. This is contrary to the truth. To read more on the myths of HRT click here... To read more on the Truth about HRT, continue on. For nomenclature clarity, there are many names for hormone therapy and while they can vary slightly, they are all referring to the same concept (with some nuanced variations) and are listed below. For simplicity, we will refer to HRT during this article.
- Hormone Therapy (HT)
- Hormone Replacement Therapy (HRT)
- Estrogen Replacement Therapy (ERT), (without progesterone)
- Menopausal Hormone Therapy (MHT)
- Bio-identical Hormone Replacement Therapy (BHRT)
What has come to light over several years through more research, clarification on old research from the WHI trials, and from larger organizations worldwide, is that women should consider HRT as single-handedly the most effective way to prevent heart disease, osteoporosis, dementia, colon cancer and to improve the quality & span of her life. These outcomes are specifically for women who begin HRT within the first 10 years from the onset of menopause, and maintain such therapy for at least this duration, if not longer.
So, let’s dive into the top 5 benefits of Hormone Replacement Therapy that you may not be aware of.
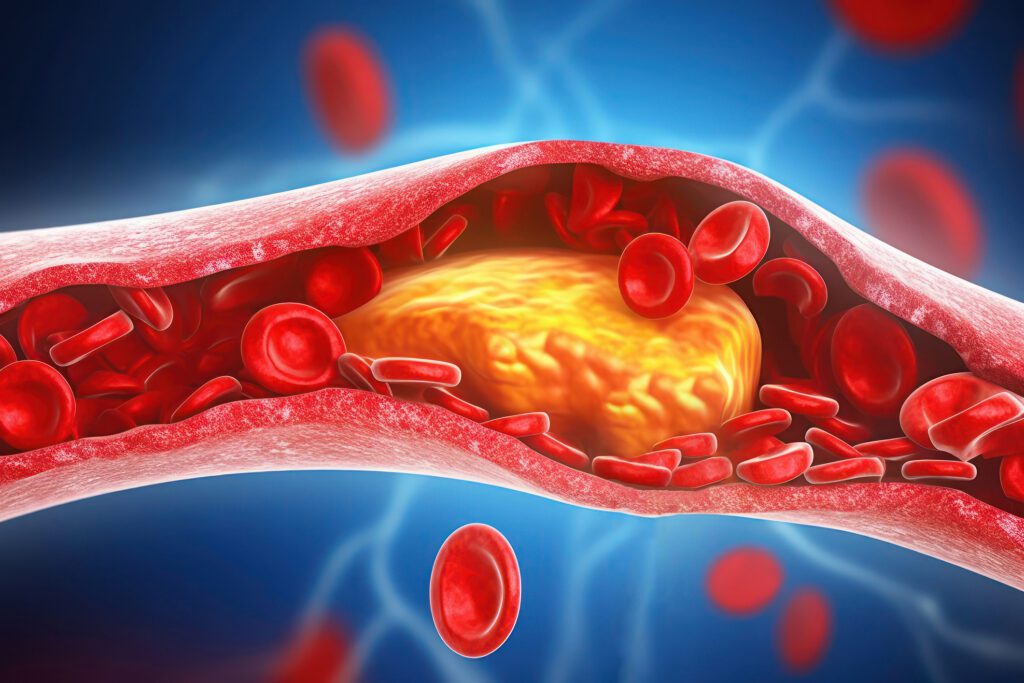
Estrogen Reduces Your Heart Disease Risk by 50%
Heart disease kills as much as 7x more women than breast cancer. Based on US data this equates to 300,000 versus 41,000 women. Being on HRT can reduce the risk of cardiovascular events and death by up to 50%.
While there are many studies – I will mention a few compelling clinical trials that provide evidence supporting the claim that hormone replacement therapy (HRT) can reduce the risk of cardiovascular events and death in postmenopausal women by up to 50%. But I will also explain why there is so much fear surrounding HRT.
The ELITE Trial known as Early versus Late Intervention Trial with Estradiol (ELITE) was a large-scale (643 females) randomized controlled trial assessing the timing hypothesis, which posits that initiating HRT closer to the onset of menopause may yield better cardiovascular outcomes.
The ELITE trial demonstrated that initiating HRT with estradiol in early menopause (within 6 years of menopause onset) was associated with improved cardiovascular outcomes compared to starting HRT later. Specifically, early initiation of HRT was linked to a significant reduction in the progression of atherosclerosis, a key factor in cardiovascular disease. While the study did not quantify the exact percentage reduction in cardiovascular events, the results suggest a substantial benefit when HRT is started early in the menopausal transition.
Another study known as the Postmenopausal Estrogen/Progestin Interventions trial (PEPI), was conducted by principal investigator Elizabeth Barrett Conner, professor of preventive medicine at the University of California in San Diego alongside Trudy Bush, an epidemiologist at John Hopkins. Together, they reviewed existing studies that concluded most, but not all, studies of HRT in postmenopausal women show around 50% reduction in the risk of a coronary event in women using unopposed oral estrogen. Furthermore, their own study of nearly 900 women found the estrogen plus progesterone was better than estrogen alone in reducing the risk of heart attacks. Preceeding these studies in 1991 cardiologist lead Goldman and statistician and Tosteson, both then at Harvard medical school, wrote a lead editorial for the new journal New England Journal of medicine titled “Uncertainty about postmenopausal estrogen. Time for action, not debate.” A consensus of epidemiological studies they wrote, had shown that women who were given post-menopausal estrogen had a 40 to 50% reduction in the risk of coronary artery disease compared with women who had not taken hormones. There are many more studies to go onto support the fact that estrogen and progesterone help prevent heart disease.
Various large-scale observational studies have investigated the effects of HRT on cardiovascular health in postmenopausal women. These studies consistently report that postmenopausal women using HRT experience a 35% to 50% lower risk of coronary heart disease (CHD) compared to non-users. For instance, a study published in the American Journal of Epidemiology found that combined postmenopausal hormone therapy was associated with a 40–50% reduction in CHD incidence among women using these preparations. These studies underscore the clear cardiovascular benefits of HRT, particularly when initiated early in the menopausal transition. Unfortunately, many medical organizations council against the use of HRT for the prevention of heart disease. This is simply a result of the ongoing dogma of the conventional medical system that continues to neglect the latest research and data. This unfortunately trickles down to the general family doctor as well. Let me explain why.
The Women’s Health Initiative (WHI) – Where We Went Wrong.
While I would prefer NOT to go down this rabbit hole, it is a necessary must, so that you can better understand WHY there is so much current-day controversy on HRT. The largest scale trial that was run on hormone therapy is known as the Women’s Health Initiative. It is fraught with problems, murky conclusions and incorrect yet sensational ideas that HRT is dangerous for you.
The Women’s Health Initiative was launched in 1991, conducted by the U.S. National Institutes of Health (NIH) and involved 161,808 postmenopausal women aged 50–79 years The purpose of the study was to assess major causes of death, disability, and frailty in postmenopausal women — particularly heart disease, breast cancer, colorectal cancer, and fractures. Three major arms of this trial included (1) 16,608 women with an intact uterus taking synthetic Estrogen + Progestin (2) 10,739 women who had a hysterectomy and were taking estrogen only therapy and (3) no hormones and continued observation. The study was cut short due to the following risks and concerns:
- The first arm was stopped early as it showed increased risk of breast cancer, stroke, and venous thrombosis. But it also showed a reduced risk of fractures and colorectal cancer. The trial stopped early due to overall harm outweighing benefits.
- The second arm was stopped early as it showed an increased risk of stroke and venous thrombosis but no increase in breast cancer, and in fact, a possible reduction in breast cancer incidence and mortality over long-term follow-up.
- The third arm continued as it was observational and later data showed timing matters — women who began HRT closer to menopause had more favourable cardiovascular and mortality outcomes – this is known as the “timing hypothesis”.
The reason for the WHI’s contradictory finding about hormones and heart disease is almost certainly that the study was not based, as they claimed, on a sample of healthy women in their late 40s and early 50s who were just entering menopause. On the contrary, not only was the median age of the women in their sample 63 years old, but fully 70% of women were seriously overweight and half were obese. Nearly 50% were either current or past cigarette smokers and more than 35% had been treated for high blood pressure. Only 10% of the women were between 50 and 54 years old, and 70% were 60 to 79, and age range where we would expect to find previously formed atherosclerotic plaques. That means that atherosclerosis was probably present in the WHI population when the study began, yet women with these well-established risk factors for heart disease were not excluded from the analysis of the effects of hormones on cardiovascular events. That is a mouthful, and while there is so much more to say on this – these very facts are why the Dogma of medicine (and its blanket claims that HRT is dangerous) prevails today and many doctors may still refuse to have an open conversation with you about your options for HRT.
According to the Framingham Heart Study, cardiovascular disease (CVD) risk approximately triples with each decade of life. This means that women in their 60s have about three times the risk of developing CVD compared to those in their 30s, and women in their 70s have about nine times the risk. This age-related increase in risk is attributed to various factors, including hormonal changes, increased prevalence of risk factors like hypertension and diabetes, and the natural aging of the cardiovascular system. It’s important to note that while age is a significant risk factor, lifestyle modifications such as maintaining a healthy diet, regular physical activity, and managing stress can help mitigate the increased risk of CVD as women age. But the evidence is clear – HRT has profound benefits.

Estrogen prevents and Delays Osteoporosis by 40%
Osteoporosis is a progressive bone disease characterized by brittle, weak bones. Having osteoporosis makes you more susceptible to bone fractures and breaks in the hip, spine or wrist. Hip fractures are especially concerning as research published in the Journal of Internal Medicine found that one in three adults age 65 and over dies within 12 months of suffering a hip fracture. That is a frightening statistic. Women are four times more likely to develop osteoporosis than men and the loss of estrogen in menopause is the most common cause. This is because estrogen performs the important role of slowing the breakdown of bone. There are estrogen receptors in bone tissue, and they need estrogen to tell them to activate formation and increase production of bone. So, when estrogen levels plummet in menopause, osteopathic bone loss is increased, and bone weakness is the result. 40 to 50% of post-menopausal women will experience a fracture related to osteoporosis during their lifetime. In addition to low estrogen, vasomotor symptoms of menopause like hot flashes and night sweats, have also been found to contribute to lower bone mineral density.
Research published in 2021, reported that estrogen therapy may help prevent bone loss and reduce the risk of fracture by 40% and its protective effect seems to have the greatest potential if it’s began within the first 10 years after menopause.
Further to this, while calcium and vitamin D supplementation is important and helpful in the reduction of bone loss in pre-menopausal women, it’s less impactful after menopause. Of course, I still recommend all my patients take Vitamin D for so many other reasons – heart health, immune health, blood glucose regulation, mood support, etc., but not as a primary prevention for osteoporosis after menopause, if there is no HRT in motion. Another hormone of interest that is still in its infancy includes testosterone therapy. Testosterone may playa role as our serum testosterone levels have been positively correlated to bone mineral density in both perimenopausal and early menopausal women. Although more research is needed in this area and it does not come without its own side effects such as acne, facial hair growth, irritability and or even hoarse voice.

Taking HRT Delays Dementia in 40-50% of Women
One of the most frustrating symptoms of menopause is a decline in executive brain function. Some call it brain fog, others feel like they are going crazy and some women report “losing their minds” and need to take a leave from work. Taking HRT can reduce a woman’s risk of developing Alzheimer’s and delaying dementia by 40 to 50%. For North American women now aged 45 – at least 20% of women are projected to develop dementia during their menopausal years and at least half of those will develop into Alzheimer’s disease. There is no non-hormonal treatment that can reverse the effects of Alzheimer’s or dementia symptoms – not medication, not the best clinical trials to-date, not exercise, not even supplements (although some of these measures may help to delay the onset). Truly – the only successful and proven intervention for the prevention of this disease in women at present – is HRT.
Across the globe, the percentages of the decreased risk of dementia and Alzheimer’s, vary quite a bit, from 24% to 65%. But they all point in the same general direction: that estrogen helps. Here are three quick summaries:
- United States: A study that followed 8,877 women in a retirement community for up to 14 years found that estrogen users had a 45% decrease of developing Alzheimer’s disease.
- Italy: a population based of 2,816 women found the estrogen users had a 70% decrease decreased risk of Alzheimer’s disease.
- Denmark: A major Danish randomized control trial, the Prospective Epidemiological Risk Factors Study, found that women randomly assigned to take HRT for 2 to 3 years had a 64% decreased risk of cognitive impairment 5 to 15 years later as compared with those on placebo who had never taken hormones.
There are naturopathic approaches that can be utilized in the prevention and prolonging of cognitive decline such as a healthy whole foods diet, regular exercise, omega three fish oils, lithium orotate, strong and healthy relationship ties and more. However, the research and evidence for these doesn’t come anywhere near the robustness of HRT. Cognitive decline and lifestyle prevention.
Estrogen Reduces Your Colon Cancer Risk by 30-50%
Colon cancer is one of the leading causes of cancer related mortality worldwide. Females also seem to have a higher prevalence of colon cancer than males. Remarkably the Women’s Health Initiative (WHI) Study demonstrated a 56% reduction in the prevalence of colon cancer following HRT treatment in post-menopausal women. Specifically, a randomized clinical trial component of the WHI found that combined estrogen plus progestin therapy was associated with a 56% reduction in colon cancer risk compared to a placebo group.
Additionally, a meta-analysis of multiple studies, including WHI data, reported that use of HRT was linked to a 38% reduction in CRC risk. These findings suggest that HRT may play a role in reducing the incidence of colorectal cancer among postmenopausal women. This suggests a protective role of estrogen therapy in colon cancer. The reasons as to why this might be may have a lot to do with the micro biome diversity in the female digestive tract. Menopause and low estrogen levels have been associated with a decrease in gut diversity, and even a slight shift toward male like bacterial composition in the intestines. HRT keeps the microbiome in check and reduces the risk of Colon Cancer by a significant margin.

HRT Increases Longevity & Life Span
Above and beyond the 4 impactful reasons already mentioned above to consider HRT, is research that suggests something even more compelling — HRT may help women live longer.Recent large-scale studies have found that women using HRT experience lower overall mortality rates compared to those who don’t. A 2020 UK retrospective cohort study followed more than 100,000 women using HRT over 30 years and found that users of combined estrogen-progesterone therapy had a 9% lower risk of death from all causes compared to non-users. In certain groups, this translated to about two additional years of life expectancy when therapy began around age 50. Another major review, a meta-analysis of 30 randomized controlled trials, found that women who started HRT before age 60 had a 39% lower risk of dying from any cause compared to those who didn’t use it. Interestingly, this survival benefit was not seen in women who began HRT later in life, suggesting once again that timing matters — starting earlier in the menopausal transition may provide the greatest longevity advantage.
What This Means for Women Considering HRT
While no study can say exactly how many years HRT might add to a woman’s life — the consistent finding is clear: women on hormone therapy tend to live longer, healthier lives, especially when therapy starts near the onset of menopause. These women also enjoy better bone density, heart health, sleep quality, and cognitive function — all factors closely tied to healthy aging.
As always, I do believe every woman should have the choice and opportunity to discuss HRT with her doctor or with any doctor who is well trained in HRT. If your doctor is unwilling to even have a conversation – then move on and find a doctor with an open mind, who is knowledgeable when it comes to HRT. While HRT isn’t for everyone, it may be for you, and you deserve to have the choice. All plans should be personalized based on your health history and risk profile. For many women, hormone therapy offers not just symptom relief — but a meaningful prevention-based approach to delaying major chronic disease while improving vitality and longevity.
References – Available upon request – only because there are too many to list. The two main sources for this article which cites all the relevant research comes from the following evidence-based books which I often recommend my patients read. These books cite all the research to support the facts of this topic.
- Estrogen Matters by Dr. Avrum Blooming, MD
- The New Menopause by Dr. Mary Claire Haver, MD