If you have Hashimoto’s hypothyroidism (HH – also called Hashimoto’s thyroiditis), you may be wondering how to lower your thyroid antibodies and manage the symptoms of thyroid dysfunction in your body.
The thyroid antibodies include both anti-thyroperoxidase antibody (TPOAb) and anti-thyroglobulin antibody (TgAb).
Many doctors seem to dismiss the presence and importance of thyroid antibodies by saying that it doesn’t affect treatment, however, there is fact-based evidence that this is definitely not true.
Not only does having thyroid antibodies present in your blood indicate you have inflammation and autoimmune disease present, it also changes the management and the treatment plan for the person affected.
First – let’s look at what autoimmune Hashimoto’s hypothyroid is and how it differs from basic hypothyroidism.
Second – I’ll briefly highlight five therapies that I’ve used successfully in patients to help them LOWER their TPO antibodies, LOWER inflammation and REDUCE autoimmune disease.
What is Autoimmune disease?
Our immune system is designed to defend the body against foreign invaders by producing antibodies that direct blood cells to destroy unwanted pathogens.
Sometimes the immune system malfunctions and attacks the body’s own cells and tissues and this is known as autoimmune disease.
Why this happens is still not clearly understood, but certainly environmental toxins, genetics and endogenous factors have been identified. Autoimmune disorders often affect blood cells and vessels, muscle and joint tissue and endocrine glands.
The thyroid gland happens to be the most commonly affected organ and is vulnerable to autoimmune disease due to its complexity.
Thyroid hormones regulate metabolism, including utilization of carbohydrates, proteins, and fats – which in turn direct cellular activity and stimulates organs including the heart and brain. In fact, the thyroid gland is your premiere metabolic hormone.
Grave’s disease and Hashimoto’s disease are both autoimmune diseases of the thyroid.
Hyperthyroidism is usually characteristic of Grave’s disease, while Hashimoto’s disease most often features hypothyroidism. In essence, the thyroid is not slow or sluggish at putting out hormones, instead our immune system has identified thyroid cells as foreign and harmful and starts to attack them.
What is especially unique to autoimmune thyroid disease verses non-autoimmune thyroid disease is that patients can fluctuate between hypothyroid and hyperthyroid symptoms and even experience symptoms of both conditions simultaneously.
So a person can initially experience irritability, anxiety, restlessness – a hyperthyroid state or a “thyroid storm” – before crashing into a hypothyroid state. What is worse, this can happen repeatedly!
Hashimoto’s hypothyroidism (HH) is the leading cause of hypothyroidism in North America.1 It is one of the most common organ-specific autoimmune disorders of the thyroid, among Graves’ disease, trophic thyroiditis, and postpartum hypothyroidism.
Hashimoto’s hypothyroid symptoms are variable for a few reasons:
First
There is great variability in the level of thyroid gland destruction and disease manifestations. One study found that approximately 90% of the thyroid must be destroyed in order for the disease to display any symptoms of hypothyroidism at all.
Another study found that elevation of autoimmune antibodies may precede diagnosis of any clinical symptoms of autoimmune disease by 2 to 7 years.
Second
In addition to thyroid gland destruction, the difference in circulating antibodies present is also a factor in HH symptomatology.
There is a correlation between an increase in blood antibody levels and development from a normal thyroid state to a hypothyroid state.
However, the rate at which those who progress to displaying obvious symptoms of hypothyroidism is not dependent on specific levels of antibodies present.
As a result, this makes diagnoses more difficult and as treating physicians we need to place greater emphasis on the clinical symptoms a person presents with, regardless of lab results.
Third
The third reason why clinical symptoms in HH vary is that those diagnosed with HH have a higher incidence of comorbid autoimmune diseases. These include celiac disease, rheumatoid arthritis, vitiligo, diabetes mellitus, Addison’s disease, and pernicious anemia.
In fact, evidence supports that celiac disease is five times more common in those with HH vs. the overall population and 57% of those diagnosed with pernicious anemia have thyroid antibodies.
A further study in 2007 assessed 104 patients with HH and 184 patients with celiac and concluded that the association was bi-directional.
Symptoms of clinical Hashimoto’s hypothyroidism include:
- Goiter (enlarged thyroid gland)
- Feeling of tightness in the neck (pain is rarely observed)
- Fatigue
- Liver function tests tend to be abnormal in 50% of patients with HH. (In such cases, hypercholesterolemia, poor gallbladder tonicity, and reduced bilirubin excretion may be contributing factors)
- Reduced intestinal peristalsis and disturbances of the transepithelial ion flux can lead to constipation. Bacterial overgrowth from hypomotility can also result in diarrhea
- Dysphagia (difficulty swallowing) & decreased appetite resulting from delayed gastrointestinal motility
- Dry skin
- Cold intolerance & cold extremities
- Yellow skin
- Coarseness or loss of hair
- Hoarseness of the voice
- Ataxia (loss of balance)
- Memory & mental impairment
- Reduced concentration
- Depression
- Irregular or heavy menses & infertility
- Myalgias (muscle aches & pain)
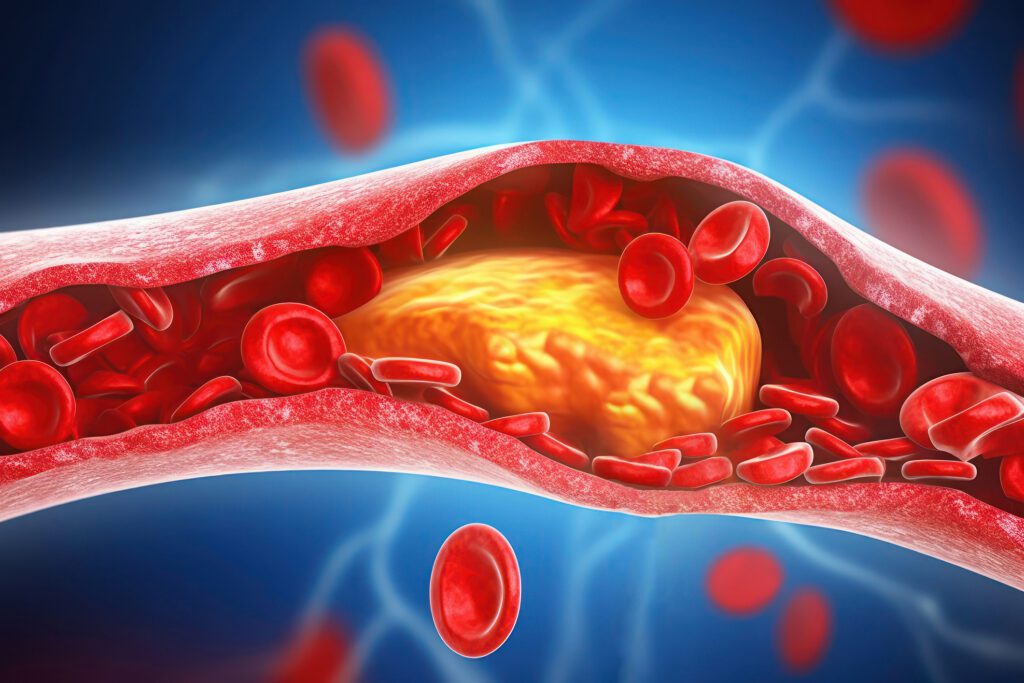
- Hyperlipidemia: Elevated cholesterol results in decreased clearance of triglycerides and elevated LDL
- Bradycardia (slow heart rate)
- Swelling & Edema – Myxedema fluid infiltration of tissues
- Possible short-term hyperthyroidism symptoms
Naturopathic Medical Treatment &
Management of Hashimoto’s Hypothyroidism
Diet, lifestyle, supplements and herbs are the cornerstone of treating any autoimmune condition. Additional bio-identical hormone repletion and low dose medications may also be needed.
ONE – Choose the right diet for your body – consider this as the necessary first step
Considering that HH has been linked to malabsorption and celiac disease, any thyroid patient with antibody levels should always eliminate gluten from their diet, no matter what dietary program you follow. While diet alone is usually not enough to lower antibodies completely, it will always help.
I must repeat, this is not a gentle “avoid gluten” recommendation, this is an absolute must!
Avoiding major food allergens and food sensitivities are helpful in decreasing allostatic load and lowering the inflammatory response in the body.
A 28-Day Elimination Diet – guided by your naturopathic physician can be helpful. This is a more comprehensive elimination diet of the major food allergens that include gluten, eggs, dairy, soy, sugar, caffeine, and all processed foods.
In addition, food allergy and sensitivity testing will help to identify inflammatory foods your body reacts to directly. By reducing these foods in your diet, you reduce the immune complexes floating around in your blood stream and thus inflammation goes down.
Finally, many patients have found the Autoimmune Paleo Diet to be helpful in reducing TPOAb. The AIP diet has gained a lot of popularity across multiple web and social media platforms because it can be so effective, but it certainly is not recommended for EVERY patient. It is a very restrictive diet (basically paleo without nuts or nightshades) and can be difficult to follow and maintain.
TWO – Treating with Nutrients and Botanicals
Nutrient deficiencies have been associated with general thyroid dysfunction and include selenium, iodine, iron, zinc, vitamin A, vitamin D and vitamin B12 among others.
Clinical evidence supports the most notable herbs to be helpful in autoimmune hypothyroid include Rosemarinic Acid, Commiphora mukul and Iris versicolour. While there are many, we will discuss just a few below.

Vitamin D
Vitamin D3 deficiency is common in general, given where we live. While Kelowna is touted for its summer sunshine – living above the 49th parallel (our Canadian border) – puts us all at an increased risk of vitamin D deficiency.
Low Vitamin D levels are found consistently in Hashimoto’s disease and in other autoimmune conditions. Vitamin D3 supplementation is suggested for both autoimmune hypothyroid and hyperthyroid disease, due to the immunomodulatory effects of vitamin D3 and the association of vitamin D3 deficiency with many autoimmune diseases.
While testing your Vitamin D levels in British Columbia is not free (it can range from $85 to $105 with an MD or an ND), dosage is often recommended based on your serum levels tested.
When treating patients with vitamin D3, blood concentrations of 25(hydroxy)vitamin D should be monitored to ensure that sufficiency is achieved and that vitamin D-induced hypercalciuria (>150 ng/mL) does not occur.
Zinc & Selenium
Have you looked at your fingernails lately? Take a peak. If you see any white spots, or more than just one – you likely have a mineral deficiency. Zinc is the most common mineral deficiency and critical for thyroid and immune function.
- Zinc acts as a powerful antioxidant
- Zinc boosts the immune system as a critical co-factor
- Zinc acts as an anti-inflammatory agent
- Zinc helps boost T4 to T3 conversion, and
- Zinc can help reduce oxidative stress
Selenium helps to boost the immune function and lower TPO antibody levels as well as increase T4 to T3 conversion.
This particular pathway to get from T4 hormone in the thyroid gland converted to T3 hormone in the liver is a metabolically demanding process and thus often low in many patients.
Two to three brazil nuts a day can easily meet your recommended daily dose of selenium – but the challenge is find these nuts organic and free of mold.
Rosemarinic Acid is derived from the lamiaceae family of plants that include rosemary, sage, basil and others. Rosemarinic Acid is well-known to reduce TPO levels. Is does so by inhibiting T cell activation and proliferation.
Above and beyond, Rosemarinic acid is also known to induces T cell apoptosis (cell death) of only actively-proliferating T cells. Overall, this plant extract drives T cell activity and reduces inflammation in the thyroid by modulating T cell promotion of proinflammatory cytokine release.
Rather than takes all these different herbs and nutrients separately, we offer formulated thyroid support that combines the above (and more) to target thyroid antibodies while supporting healthy thyroid function.
THREE – Consider using Bio-Identical Hormone Replacement: DHEA & Progesterone
Before considering the above hormones, we always recommend dried urine hormone testing to assess your functional and ideal levels to see if supplementation is appropriate for you.
DHEA can be very helpful in reducing antibody levels. The majority of patients who have Hashimoto’s are women. This is actually true of almost all autoimmune disease (with few exceptions).
Part of the reason this is thought to occur has to do with lower levels of testosterone and DHEA – our male “androgen” hormones. The less testosterone you have, the more likely you are to develop autoimmunity and Hashimoto’s hypothyroidism.
In my experience of testing many patients with Hashimoto’s, I can attest that the vast majority also have low testosterone levels in addition to low DHEA levels. Adding these androgens to your treatment regimen (or adding in herbs to help build them) can help in the following ways:
- Balance TH1 and TH2 immune response
- Lower autoimmunity in the body (in some cases, suppresses it).
- Boost weight loss & Increases sex drive
Progesterone is always helpful for multiple reasons. Alone, progesterone offers anti-inflammatory benefits, promotes deeper sleep, calms the nervous system, supports thyroid and adrenal function in general. Progesterone hormone is often over-looked and under-tested in conventional medicine
NOTE: Hormone testing is a good idea, to help guide in dosing. While simple serum hormones can be ordered (free and total Testosterone, DHEA-s and Progesterone), urine hormone testing offers more advantages:
- Collecting over a full day helps to capture a true average value. A blood test may capture your highest or lowest level of the day, as our hormones pulse every few hours.
- Pathways and metabolites are provided so you can see where your hormones flow to and what pathways may be stuck or hindered – this can reveal – what nutrients and enzyme need to be repleted to move through smoothly and resolve symptoms
- Additional B vitamin status, adrenal function, melatonin and methylation markers are often included and provide a “whole picture” approach to your hormone health and underlying thyroid concerns

FOUR – Improve your Gut Function
When you have hypothyroidism, digestive issues are almost always part of the picture. In addition to the necessary dietary recommendations above, the gastrointestinal issues I’m specifically referring to are two very common and under diagnosed conditions in hypothyroidism:
- SIBO or Small Intestinal Bacterial Overgrowth
- Yeast Overgrowth
As many as 54% of people may have this condition and likely don’t even know it! Symptoms include:
- Gas or Bloating – especially 30-60 minutes after a meal
- Chronic constipation
- History of vaginal yeast infections or Intestinal yeast overgrowth
- History of acid reflux
- History of diabetes or concurrent peripheral neuropathy (numbness or tingling)
- History of vagal nerve dysfunction
It is possible to repair your gut health naturally, with naturopathic treatment. Digestive restoration is possible and you can restore balance in the body. SIBO can be diagnosed in our clinic with a simple breath test which tests for certain gasses from unhealthy gut bacteria.
Likewise, yeast overgrowth can be diagnosed with a simple in-clinic test.
We take a 5 step approach to treating gut health for patients suffering from both yeast overgrowth and SIBO. This treatment process consists of what we call the 5 R’s:
- Remove certain foods and stressors to your GI tract
- Replace harmful yeast and bacteria with digestive enzymes you are deficient in
- Re-inoculate and help good bacteria thrive with probiotics and other vitamins and supplements
- Repair the digestive tract after the damage with additional vitamins and minerals
- Rebalance the body and calm your nervous system by following a routine to promote healing
Once your gut health has been restored, your GI tract will be much better able to process foods. This side effect of hypothyroidism can be repaired with consistent treatment and dietary changes.
FIVE – LDN Therapy – Helps improve status of the immune system overall
Low Dose Naltrexone (LDN) therapy helps to improve HH by addressing the integrity of the immune system. Based on the effectiveness of LDN in other autoimmune disorders, LDN can reduce the production of thyroid antibodies of Hashimoto’s hypothyroidism.
As LDN is able to modulate the immune system by acting on endorphin receptors, it can subdue the immune reaction and slow down the destruction of thyroid cells. I have also seen when patients take LDN who are also on thyroid replacement medication that they can often lower their hormone dosage as the immune-normalizing effects by LDN slow down the autoimmune process.
Unlike standard treatment, some patients may not have to take this medicine for a lifetime. Young patients with Hashimoto’s can go into remission through modulating your immune system with LDN. The medication will help them move towards an appropriate immune status, and once the immune system is in balance again, you may be able to discontinue the LDN.
It is important to note that LDN is considered very safe. But there are short term side effects which include nausea, sleep disturbances, vivid dreams, and irritability. These side effects normally go away over time (a few days to a few weeks) or can be eliminated by reducing the dosage or tapering the dosage slowly.
Summary
Supporting the immune system with dietary modifications, nutrients, herbs and low dose BHRT or LDN medication can all help to reduce inflammation in Hashimoto’s Hypothyroidism.
A trend of continued elevation of TPOAb and TGAb over time is concerning (especially in the face of treatment). If you fall into this category (slightly raised Ab or they are outside of the reference range) AND you also have symptoms of hypothyroidism then it’s definitely worth considering naturopathic medicine and the treatments mentioned above, as these are outside the scope and understanding of the standard medical model.
Each of these approaches has varied mechanisms of action supporting thyroid hormone homeostasis. As mentioned, removing gluten from ones diet reduces the overall immune dysfunction and inflammatory load of antibody levels; Vitamin D3 and rosemarinic acid play a role in T cell modulation and cytokine response; and so forth.
Incorporating daily techniques for reducing stress is critical as stress drives inflammation, and depletes healthy hormone levels. Improving digestion, absorption and optimizing your GI health, while ensuring proper nutrition is also important as these elements are all known to interfere with optimal thyroid function.
Lastly, I should mention the important for patients with autoimmune thyroid disease to incorporate aerobic exercise into their lifestyle.
Aerobic exercise induces 5′-deiodinase, the enzyme that stimulates peripheral production of active T3 from T4. While someone may feel too tired or unwell to incorporate exercise, starting slowly and in short durations, can still provide meaningful benefit.
When treated appropriately, restoration of normal thyroid function in early stages of autoimmune hypothyroid disease can be achieved.
References:
1. Baskin HJ, Cobin RH, Duick DS, et al, for the American Association of Clinical Endocrinologists. AACE Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002;8(6):457-469.
2. Desailloud R, Hober D. Viruses and thyroiditis: an update. Viro J. 2009;6:5.
3. Xie LD, Gao Y, Li MR, Lu GZ, Guo XH. Distribution of immunoglobulin G subclasses of anti-thyroid peroxidase antibody in sera from patients with Hashimoto’s thyroiditis with different thyroid functional status. Clin Exp Immunol. 2008;154(2):172-176.
3b. Hutfless S., Matos P Talor MV, et al. Significance of prediagnostic thyroid antibodies in women with autoimmune thyroid disease. J Clin Endocrinol Metab. 2011;96:E1466-E1471.
4. Orgentec Diagnostika GmbH. Immunometric Enzyme Immunoassay for the quantitative determination of antibodies against thyroglobulin (TG). http://www.orgentec.com/user_images/73/307576124_502e.pdf. Updated August 2005. Accessed February 11, 2010.
5. Calgar E, Ugurlu S, Ozenoglu A, Can G, Kadioglu P, Dobrucali A. Autoantibody frequency in celiac disease. Clinics (Sao Paolo). 2009;64(12):1195-1200.
6. Hadithi M, de Boer H, Meijer JW, et al. Coeliac disease in Dutch patients with Hashimoto’s thyroiditis and vice versa. World J Gastroenterol. 2007;13(11):1715-1722.
7. Duntas LH. Does celiac disease trigger autoimmune thyroiditis? Nat Rev Endocrinol. 2009;5(4):190-191.
8. Kon YC, DeGroot LJ. Painful Hashimoto’s thyroiditis as an indication for thyroidectomy: clinical characteristics and outcome in seven patients. J Clin Endocrinol Metab. 2003;88(6):2667-2672.
9. Greenfield JR, Samaras K. Evaluation of pituitary function in the fatigued patient: a review of 59 cases. Eur J Endocrinol. 2006;154(1):147-157.
10. Daher R, Yazbeck T, Jaoude JB, Abboud B. Consequences of dysthyroidism on the digestive tract and viscera. World J Gastroenterol. 2009;15(23):2834-2838.
11. Delange F. The disorders induced by iodine deficiency. Thyroid. 1994;4:107-128.
12. Pizzulli A, Ranjbar A. Selenium deficiency and hypothyroidism: a new etiology in the differential diagnosis of hypothyroidism in children. Biol Trace Elem Res. 2000;77:199-208.
13. Watts DL. The nutritional relationships of the thyroid. Journal of Orthomolecular Medicine. 1989;4:165-169.
14. Safran M, Paul TL, Roti E, Braverman LE. Environmental factors affecting autoimmune thyroid disease. Endocrinol Metab Clin North Am. 1987;16:327-342.
15. Stangl GI, Schwarz FJ, Kirchgessner M. Cobalt deficiency effects on trace elements, hormones and enzymes involved in energy metabolism of cattle. Int J Vitam Nutr Res. 1999;69:120-126.
16. Tamer G, Arik S, Tamer I, Coksert D. Relative vitamin D insufficiency in Hashimoto’s thyroiditis. Thyroid. 2011;21(8):891-896.
17. Watson RR, ed. Handbook of Vitamin D in Human Health: Prevention, Treatment and Toxicity. Wageningen Academic Publishers; 2013.
18. J Clin Endocrinol Metab. 2002 Apr;87(4):1687-91.