Do you suffer from frequent painful headaches? Is it necessary to go into a dark room, close the door, silence the world and bury your head under a pillow for several hours? If this sounds familiar – and you have not found a way to reduce and eliminate your migraine headaches – you should consider seeing a Naturopathic Doctor.
Migraine headaches are often challenging to treat due in part to their multiple underlying causes. It is well-known that specific foods – and even certain classes of foods – trigger migraine attacks in some patients. And when you remove inflammatory foods, the migraines can resolve.
A 2017 observational study of 115 children with chronic headaches excluded specific foods (including caffeine, MSG, cocoa, aspartame, and others) for six weeks.0 At the six-week mark, 87% of the children no longer suffered from headache.0
I recommend food sensitivity and food allergy testing as a useful tool for reducing the severity and frequency of migraine headaches.
the difference between “food allergy” and “food sensitivity”
First, it is important to clarify the difference between food sensitivities and food allergies. Food sensitivities are NOT food allergies.
A food allergy is a potentially serious health condition triggered by the release of IgE antibodies to a specific food. Food allergy symptoms typically appear very soon (within a few minutes to a few hours) after eating a problem food (e.g. peanuts). Food allergy reactions may include a condition called anaphylaxis, which can be life-threatening; hives (red swollen patches on skin); breathing difficulties, vomiting or diarrhea and other symptoms. It is possible to measure IgE antibodies in the blood. A food allergy is scientifically referred to as an IgE Type I hypersensitivity reaction and while it is only a small (5-10%) percentage of immune cells, reactions can be severe and life-threatening for some people.
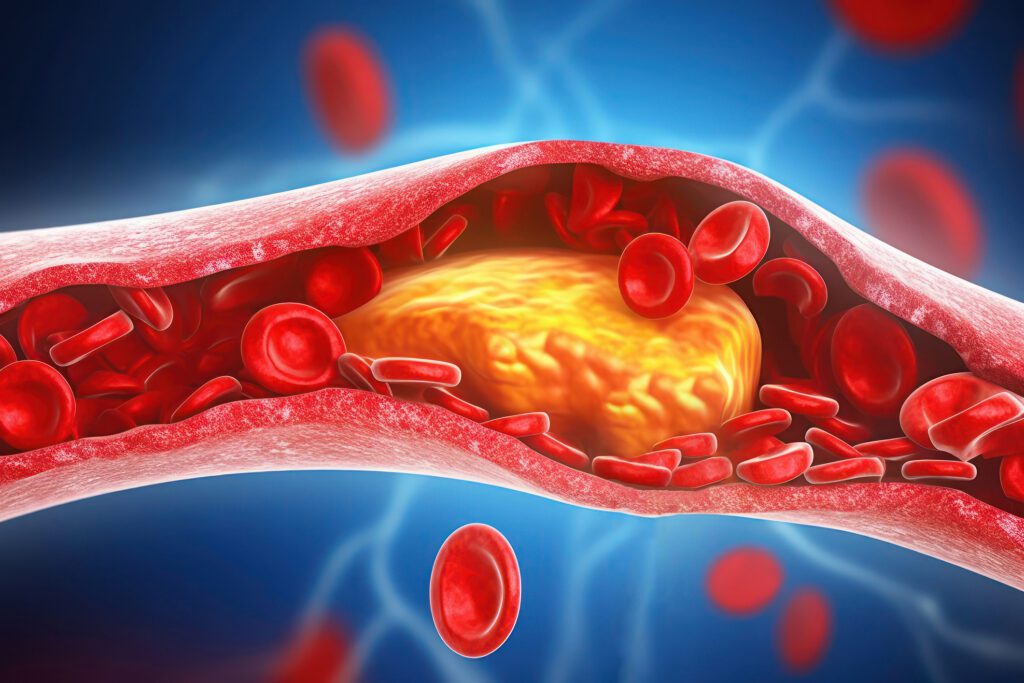
A food sensitivity typically takes months to develop and is triggered by IgG antibodies. Food sensitivity reactions can take several hours to several days to develop and they are low-grade and difficult to detect. The release of IgG antibodies to specific foods is considered normal, as is the formation of antigen-antibody complexes (which form when a food antigen meets an IgG antibody and they bind together). 1 In a healthy functioning immune system, cells called macrophages typically remove these complexes; however, when many antigen-antibody complexes are present, macrophages may not be able to remove them all. The complexes that are left behind deposit in tissue and release substances that promote inflammation.² Inflammation is much more likely to occur if the reactive food remains a regular part of the diet since more immune complexes will form, and in turn may trigger inflammation and contribute to inflammation, headache and migraines.
Let’s dive into a little more research, shall we?
A clinical double-blind, randomised, cross-over trial conducted in 2010, looked at IgG food sensitivity testing in 30 patients with migraine headaches without aura. Patients were tested for IgG antibodies against 266 food antigens detected via an ELISA blood test. Patients started a regular diet for the first 6 weeks and were then randomised to a 6-week diet either abstaining from or including specific foods with raised IgG antibodies. Both patients and their doctors were blinded to IgG test results and the type of diet (provocation or elimination). Primary parameters measured the number of headache days and migraine attack count. Of 30 patients, 28 were female and 2 were male, aged 19-52 years (mean, 35 +/- 10 years).
The IgG food reactions tested produced an average of 24 positive IgG food sensitivities (+/- 11) out of 266 foods. Results showed a significant reduction in the number of headache days: from 10.5 headache days (+/- 4) down to 7.5 headache days (+/- 3.7) with a P < 0.001, and; the number of migraine attacks also reduced from 9.0 days (+/- 4.4) down to 6.2 (+/- 3.8) with a P < 0.001 in the elimination diet period.3
This study shows that diet restriction based on IgG antibody testing & dietary elimination – in as little as 6 weeks – is an effective strategy in reducing the frequency of migraine attacks.
Another Study out of Mexico tested serum antibodies to specific 108 IgG food allergens by enzyme immunoassay from 56 patients with migraine and a control group without migraine. Again, results showed that in addition to statistical significant differences in the number of positives for IgG food allergens between patients with migraine and a controlled group, elimination diets successfully controlled the migraine without the need of medications. The conclusion of this study was to recommend serum IgG antibody testing to common foods in patients with migraine headaches.4
Large Study Identifies Food Sensitivity Testing & Removal LeD to Symptom Relief
The British Allergy Foundation (known as Allergy UK) commissioned a study of patients who had recently received an IgG food sensitivity test (within the previous 3 months). The goal of the study was to find out whether removing reactive foods from the diet improved patients’ symptoms. The results were published in Nutrition & Food Science in 2007.12 Of the over 5000 patients included, 70% rigorously followed the results and eliminated all their reactive foods.
Patients who successfully removed reactive foods from their diets saw improvement in a variety of symptoms, most within 3 weeks. Symptom improvement was shown to be directly related to the removal of the reactive foods as symptoms returned when the reactive foods were reintroduced into the diet.
- 76% saw significant symptom improvement
- 68% saw benefit within 3 weeks
- 92% had symptoms return when reactive food were added back to the diet
Symptom relief varied by body system, with digestive symptoms like irritable bowel syndrome and psychological symptoms like anxiety and depression, showing the greatest improvement when reactive foods were removed.
Published research also shows the benefits of removing IgG-reactive foods for several other health conditions. They include: functional dyspepsia (indigestion)9, Crohn’s disease (a serious type of inflammatory bowel disease),15 and Sjögren’s syndrome,16 an immune disease.
In Summary
Many patients who suffer from migraines or chronic headaches will often improve once food triggers are tested and removed from the diet. While migraine headaches are often the result of multiple underlying causes (inflammation, mitochondrial dysfunction, stress, hormonal imbalance, etc.), food identification and removal is a reasonable and effective first choice for pain reduction.
Food sensitivities are very different from food allergies. The symptoms associated with food sensitivities develop slowly over time as IgG antibody-food antigen immune complexes deposit in various parts of the body and trigger inflammatory reactions. Depending on where the immune complexes deposit, inflammation can contribute to a variety of different health conditions.
Numerous studies in peer-reviewed journals have shown the health benefits of removing IgG reactive foods, particularly for migraine headaches,3,4 and irritable bowel syndrome,5,6,7,8,9,10 and even weight management.13,14,17 There is good evidence that most patients experience improvement in symptoms when IgG reactive foods are removed from the diet.12
Mind Body Soul Integrative Clinic only uses reputable, industry-leading laboratories for food sensitivity testing and food Allergy testing. Our labs include Alletess Labs, Meridian Valley Labs, Great Plains Laboratory, Rocky Mountain Analytical and US Biotek .
We have 4 Naturopathic Doctors on staff to offer in-house blood draws at the end of your naturopathic visit, should this type of testing be indicated for your health concerns.
References:
0. Taheri S. Effect of exclusion of frequently consumed dietary triggers in a cohort of children with chronic primary headache. Nutr Health. 2017;23(1):47-50. doi:10.1177/0260106016688699
1. Gocki J, Bartuzi Z. “Role of immunoglobulin G antibodies in diagnosis of food allergy.” Adv Dermatol Allergol Vol.33 No..4 (2016): 253-56.
2. Janeaway, CA Jr, Traver P, Walport M et al. Immunobiology: The Immune System in Health and Disease. 5th ed. New York: Garland Science, 2001. Print.
3. Alpay K, Ertas M, Orhan EK et al. «Diet restriction in migraine, based on IgG against foods: a clinical double-blind, randomised, cross-over trial.” Cephalalgia Vol. 30.No. 7 (2010): 829-37. PMID: 20647174
4. Arroyave Hernández CM1, Echavarría Pinto M, Hernández Montiel HL. “Food allergy mediated by IgG antibodies associated with migraine in adults.” Rev Alerg Mex. 2010 Mar-Apr;57(2):49. PMID: 18693538
5. Aydinlar EI, Dikmen PY, Tiftikci A et al. “IgG-Based Elimination Diet in Migraine Plus Irritable Bowel Sydrome.” Headache. (2012): 1-12.
6. Atkinson W, Sheldon TA, Shaath N et al. “Food elimination based on IgG antibodies in irritable bowel syndrome: a randomized controlled trial.” Gut. Vol. 53 (2004): 1459–1464.
7. Drisko J, Bischoff B, Hall M et al. “Treating Irritable Bowel Syndrome with a Food Elimination Diet Followed by Food Challenge and Probiotics.” JACN Vol. 25.No. 6 (2006): 514-22.
8. Aydinlar EI, Dikmen PY, Tiftikci A et al. “IgG-Based Elimination Diet in Migraine Plus Irritable Bowel Sydrome.” Headache. (2012): 1-12.
9. Zuo XL, Li YQ, Li YJ et al. “Alterations of food antigen-specific serum immunoglobulins G and E antibodies in patients with irritable bowel syndrome and functional dyspepsia.” Clin Exper Allergy. Vol. 37 (2007): 823-30.
10. Kalliomaki, MA. “Food allergy and irritable bowel syndrome.” Curr Opin Gastroen. Vol. 21 (2005): 708-711.
11. Mansueto P, D’Alcamo A, Seidta A, et al. . “Food allergy in irritable bowel syndrome: The case of non-celiac wheat sensitivity.”World J Gastroenterol. Vol. 21 No.23 (2015):7089-7109.
12. Hardman G, Hart G. “Dietary advice based on food-specific IgG results.” Nutr Food Sci Vol. 37.No. 1 (2007): 16-23.
13. Wilders-Truschnig M, Mangge M, Lieners,C et al. “IgG antibodies against food antigens are correlated with inflammation and intima media thickness in obese juveniles.” Exper Clin Endocrinol Diabetes Vol. 116.No. 4 (2008): 241-45.
14. Lewis JE, Woolger JM, Mellilo A, et al. “Eliminating Immunologically-Reactive Foods from the Diet and its Effect on Body Composition and Quality of Life in Overweight Persons.” J Obes Weig los Ther Vol. 2.No. 1 (2012): 1-6.
15. Bentz S, Hausmann M, Piberger H et al. “Clinical relevance of IgG Antibodies against Food Antigens in Crohn’s Disease: a Double-Blind Cross-Over Diet Intervention Study.” Digestion. Vol. 81 (2010): 252-264.
16. Kim-Lee C, Suresh L, Ambrus JL. “Gastrointestinal disease in Sjogren’s syndrome: related to food hypersensitivi- ties.” SpringerPlus. Vol. 4.No. 766 (2015): 1-5.
17. Onmus MY, Avcu EC, Saklamaz A. “The Effect of Elimination Diet on Weight and Metabolic Parameters of Over- weight or Obese Patients Who Have Food Intolerance” J Food Nutr Res. Vol. 4 No.1 (2016):1-5.